Exploring Common Eye Diseases: A Guide by Ophthalmology Associates
Posted by: Ophthalmology Associates of Fort Worth in Cataract Surgery

“What you see is what you get.”
It’s a common saying that you should see everything as it is, with nothing hidden. This applies to your eyes, too.
Your eye health determines what you can see. Eye health is a crucial aspect of overall wellness, often overlooked until noticeable problems arise.
Millions suffer from various eye diseases all over the world. In Texas alone, many people have problems with their eye health, which impacts their quality of life.
These can range from mild irritations to severe vision loss, highlighting the importance of ocular health through regular check-ups.
In this article, we’ll discuss eye diseases most commonly experienced, their symptoms, treatments, and preventative measures offered by the eye experts, Ophthalmology Associates.

Understanding Common Eye Diseases
By definition, common eye diseases and disorders refer to a range of conditions that can impair vision and the overall health of your eyes.
These conditions vary from easily treatable and preventable concerns to more serious ones that can lead to vision problems or blindness.
The most prevalent among these are cataracts, glaucoma, macular degeneration, and diabetic retinopathy, especially among older people.
These diseases can affect your ability to perform daily activities, maintain independence, and enjoy a high quality of life.
Luckily, these conditions can be managed effectively with early diagnosis, making regular eye examinations an important part of your health checkups.
Age-Related Macular Degeneration (AMD)
Age-Related Macular Degeneration (AMD) is a common eye disease characterized by the deterioration of the macula, the part of the retina responsible for sharp, central vision.
As the name suggests, this condition is primarily age-related and is a leading cause of vision loss among people older than 50.
Below are two types of AMD:
Dry AMD
The more common type of AMD occurs when the macula breaks down and gets thinner over time, causing tiny lipid deposits to form under the retina.
This results in blurred or distorted vision or black spots.
Wet AMD
On the other hand, wet AMD is not as common but is more severe than Dry AMD.
This occurs when abnormal blood vessels grow under the retina, leaking fluid and blood. This causes the macula to get scarred and damaged.
Symptoms may appear as any of the following:
- Sudden or rapid loss of central vision
- Straight lines appearing wavy or distorted
- Dark spots or blind spots in the central vision
Wet AMD can progress quickly and can result in serious vision problems if not treated early.
Risk Factors for AMD
AMD risk factors include:
- Advancing age
- Genetics
- Lifestyle choices, such as smoking and poor diet.
- Obesity and high blood pressure can also increase the chances of AMD.
Symptoms
AMD symptoms often develop gradually and can include the following:
- A blurry or blind spot in the center of the field of vision
- Visual distortions
- Reduced central vision in one or both eyes
- Changes in color perception.
AMD’s progression can vary, and Dry AMD can turn into Wet AMD.
Treatment
Depending on the type and severity, AMD has various treatment options.
There is no cure for dry AMD. However, a healthy diet rich in antioxidants, vitamins, and minerals can slow its progression.
On the other hand, Wet AMD can be treated more aggressively with anti-VEGF (Vascular Endothelial Growth Factor) medication injections that inhibit the growth of abnormal blood vessels in the eye.
In some cases, laser therapy and photodynamic therapy are also an option. While these treatments can be effective in disease control, they cannot cure AMD.
Preventing AMD
To prevent AMD, an eye doctor will suggest strategies focused on lifestyle changes like:
- Regular exercise
- Maintaining a healthy weight
- Quitting or not smoking
- Eating a balanced diet rich in green, leafy vegetables and fish
Protecting your eyes from ultraviolet light with sunglasses outdoors is also essential. Undergoing regular eye exams is also crucial for detecting early symptoms and management of AMD.
Glaucoma
Glaucoma is characterized by damage to the optic nerve, the part of the eye that sends visual information to the brain.
The damage is usually a result of increased intraocular pressure (IOP) but can also occur with normal or even low IOP. If left untreated, glaucoma can lead to irreversible vision loss and blindness.

There are different types of glaucoma, including:
Primary Open-Angle Glaucoma (POAG)
- It’s the most common type and develops gradually without pain and noticeable symptoms at the early stages, thus referred to as a “silent thief of sight.”
- The increased fluid pressure inside the eye causes the damage.
- Symptoms are the loss of peripheral vision at the later stages.
Angle Closure Glaucoma
- With this type of glaucoma, the iris bulges forward, partially or entirely blocking the eye’s drainage angle, causing IOP.
- Compared to POAG, this type can develop without warning. It’s considered a medical emergency and requires immediate treatment to prevent permanent vision loss.
- Symptoms are severe pain, redness, blurred vision, and halos around lights.
Normal-Tension Glaucoma (NTG)
- A common type of glaucoma where the optic nerve is damaged even when eye pressure is at a normal range.
- It progresses slowly and may not cause vision loss for a long time.
- NTG has no noticeable symptoms at the early stages, similar to POAG.
Glaucoma Treatment
The best glaucoma treatment for patients will depend on factors like the type of glaucoma, its severity, and other personal preferences.
Below are the different treatment options for patients with glaucoma:
- Medication: It’s the most common option, usually as prescription eye drops. This works by reducing fluid production in the eye or improving fluid drainage.
- Laser surgery: Laser procedure treatments decrease eye pressure by creating new drainage channels for Angle Closure glaucoma or widening existing ones for POAG.
- Surgery: If other treatments fail, traditional surgical procedures can be an option, especially for more advanced cases. In surgical procedures, eye doctors create a new pathway for fluid to drain from the eye.
While treatment is available, vision loss due to glaucoma is irreversible. This is why regular eye exams are crucial for detecting glaucoma, especially since symptoms may not always appear at the early stages.
Get expert glaucoma treatments from Ophthalmology Associates. Find out more here.
Cataracts
Cataracts happen when the eye’s natural lens becomes cloudy, leading to problems with seeing clearly. It’s one of the most common eye problems primarily caused by the following:
- Aging, as the proteins in the eye’s lens break down over time
- Genetics as some individuals can be more predisposed to cataracts than others
- Environmental factors like prolonged exposure to ultraviolet light, smoking, and diabetes.
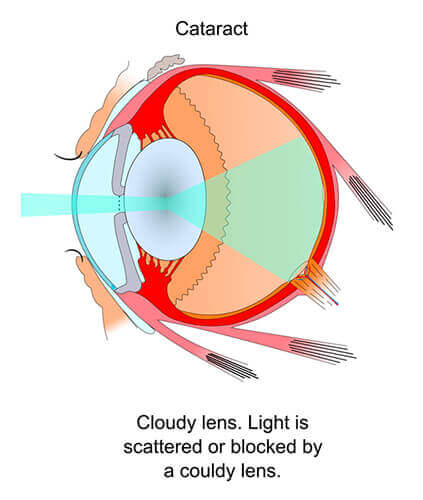
Symptoms
Cataracts may cause different symptoms. If left untreated, they can progress, significantly lowering one’s quality of life.
Symptoms include:
- Cloudy or blurred vision
- Poor vision at night
- Sensitivity to light and glare
- Seeing “halos” around lights
- Constantly changing prescription glasses
- Fading or yellowing of colors
Diagnosing Cataracts
To diagnose cataracts, patients need to undergo a comprehensive eye examination. This includes a visual acuity test, pupil dilation, and a slit-lamp examination.
Monitoring the progression of cataracts is crucial to determine the right time for surgical intervention.
Cataracts Treatment
Cataracts can be removed through surgery, a standard procedure with a high success rate. Here, the cloudy lens is removed and often replaced with a clear artificial lens called an intraocular lens (IOL).
Various types of IOLs are available, and the choice depends on the patient’s needs and the surgeon’s advice.
Another essential way to prevent or potentially slow the progression of cataracts is to adopt certain lifestyle changes, such as:
- Wearing sunglasses to block ultraviolet sunlight
- Quitting smoking
- Reducing alcohol consumption
- Eating a diet rich in vitamins and antioxidants
- Properly managing other health conditions like diabetes
Visit our website for more detailed information on managing and treating cataracts.
Diabetic Retinopathy
Diabetic retinopathy is a diabetes-related condition that affects the eyes. This eye problem is caused by damage to the retina’s blood vessels, the light-sensitive tissue at the back of the eye.
This can develop in anyone who has type 1 or type 2 diabetes. The chances of getting this complication become higher the longer someone has diabetes and the less controlled their blood sugar is.
Risk Factors
Key risk factors for diabetic retinopathy are:
- Poor control of blood sugar levels
- Prolonged duration of diabetes
- High blood pressure and cholesterol levels.
- Smoking
- A family history of diabetes or diabetic retinopathy
Stages of Diabetic Retinopathy
Below are the different stages of this condition:
- Mild Non-Proliferative Retinopathy: This is the early stage in which small balloon-like swellings appear in the retina’s blood vessels.
- Moderate Non-Proliferative Retinopathy: The retina’s blood vessels become blocked.
- Severe Non-Proliferative Retinopathy: More blood vessels are blocked, depriving several areas of the retina of their blood supply. This triggers the body to grow new blood vessels for nourishment.
- Proliferative Diabetic Retinopathy (PDR): At this advanced stage, the body grows new blood vessels that are weak and can leak or bleed, leading to serious vision problems or blindness.
At the different stages, the impact can vary from mild vision problems to severe vision loss and blindness.
Diabetic patients must undergo regular eye exams for early detection, monitor their progression, and take the necessary steps to prevent severe consequences.
Treatment Options
There are different treatment options for the advanced stages of diabetic retinopathy. These can include:
- Laser therapy: This procedure shrinks or stops the growth of new blood vessels
- Injections: Medications injected into the eye to stop inflammation or blood vessels from leaking.
However, the best way to prevent or slow diabetic retinopathy is to effectively manage diabetes by controlling blood sugar levels, blood pressure, and cholesterol.
Dry Eye Syndrome
Dry Eye Syndrome is one of the most common eye conditions when the eyes don’t produce enough tears or when the tears evaporate too quickly.
When this happens, the eye’s surface gets inflamed and damaged. Several factors contribute to this condition, including:
- Age: The risk increases with age, particularly in individuals over 50.
- Gender: Women are more likely to suffer from Dry Eye Syndrome due to hormonal changes associated with pregnancy, the use of oral contraceptives, and menopause.
- Environmental Factors: Wind, dry air, and prolonged screen time can cause tear evaporation, while smoke and dust can irritate the eyes.
- Medical Conditions: Sjögren’s syndrome, rheumatoid arthritis, and diabetes can influence tear production.
Additionally, eyelid problems or wearing contact lenses for too long can contribute to dry eyes.
Symptoms
Below are the most common symptoms of Dry Eye Syndrome:
- Persistent dryness
- A burning or scratchy sensation in the eyes
- Light sensitivity
- Eye redness
- Blurred vision
- That feeling of having something in your eyes
Meanwhile, some individuals may experience excessive tears as a response to the dryness and irritation.
Treatment Options
The main objective of Dry Eye Syndrome treatment is to restore or maintain the average amount of tears to minimize dryness and related discomfort. Options include:
- Artificial Tears: Using over-the-counter eye drops to supplement natural tear production.
- Lifestyle Changes: Increasing humidity levels at home or work, taking regular screen breaks, and wearing sunglasses outdoors.
- Prescription Medications: Taking anti-inflammatory medications or eye drops that increase tear production.
In more severe cases, certain procedures might be required to block the tear ducts to reduce tear loss. Another method is to use special contact lenses that protect the eye’s surface and trap moisture.
If you have Dry Eye Syndrome, it is essential to follow a tailored treatment plan and make the necessary lifestyle adjustments.
Staying hydrated, eating a diet rich in omega-3 fatty acids, and maintaining good eyelid hygiene can manage and prevent symptoms.
Visit our website for information on our treatment options for Dry Eye Syndrome.
Safeguarding Your Vision for a Brighter Tomorrow
Understanding the causes and symptoms of common eye diseases is fundamental to maintaining good vision.
Each condition presents distinct challenges, but early detection and treatment can significantly mitigate their impact on your eyesight and quality of life.
By prioritizing eye health through regular exams, you can catch potential issues before they become more severe.
At Ophthalmology Associates, we provide the best and most comprehensive eye care tailored to your needs.
We strongly encourage you to schedule regular eye examinations to keep your eyes healthy.
Contact us now to schedule your eye exam, or you can visit our offices in Texas.
